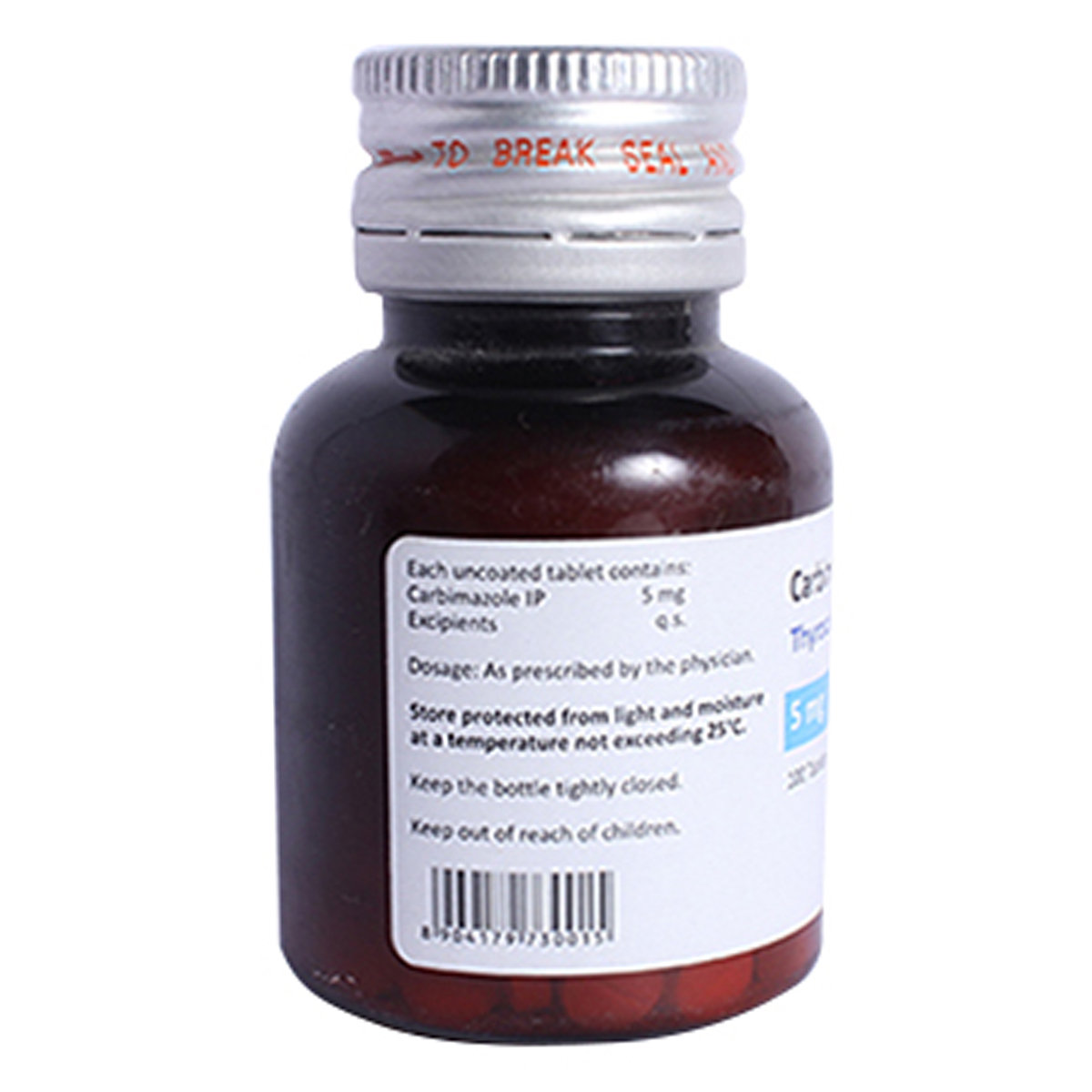
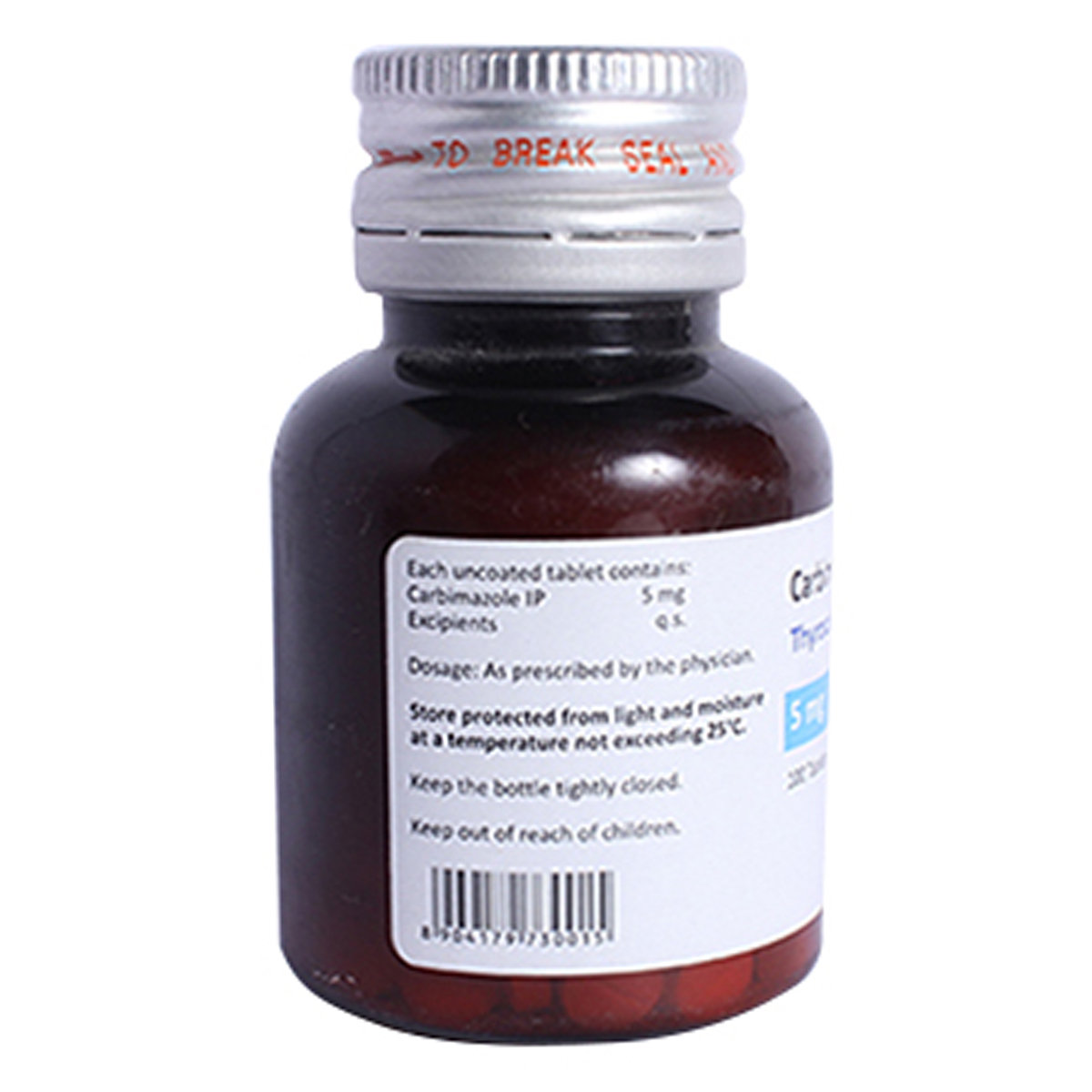
THYROCAB 5MG TABLET
MRP ₹229.5
(Inclusive of all Taxes)
₹34.4 Cashback (15%)
Provide Delivery Location
Online payment accepted
 Prescription drug
Prescription drugWhats That
Composition :
Manufacturer/Marketer :
Consume Type :
Expires on or after :
Return Policy :
NPPA :
About THYROCAB 5MG TABLET
THYROCAB 5MG TABLET belongs to a class of drugs called anti-thyroid agents used in the treatment of hyperthyroidism (overactive thyroid gland). Hyperthyroidism is a condition in which the thyroid gland produces excessive thyroxine hormone. It increases metabolism and causes unintentional weight loss.
THYROCAB 5MG TABLET contains Carbimazole that works by decreasing the production of thyroid hormones by the thyroid gland. Thus, it balances the levels of thyroid hormones.
Take THYROCAB 5MG TABLET as prescribed by your doctor. You are advised to take THYROCAB 5MG TABLET for as long as your doctor has prescribed it for you based on your medical condition. In some cases, you may experience headache, dizziness, nausea, skin rash, itching, joint pain, changes in taste or hair thinning. Most of these side effects of THYROCAB 5MG TABLET do not require medical attention and gradually resolve over time. However, if the side effects persist or worsen, please consult your doctor.
If you are known to be allergic to THYROCAB 5MG TABLET or any other anti-thyroid medicines, please tell your doctor. THYROCAB 5MG TABLET is not recommended for children below 2 years of age. If you are breastfeeding, avoid taking THYROCAB 5MG TABLET as it may be excreted in breast milk in small amounts and harm the unborn baby. Please consult a doctor if you are pregnant or planning for pregnancy before taking THYROCAB 5MG TABLET. You are recommended to use effective contraceptive measures while taking THYROCAB 5MG TABLET to avoid pregnancy. Drive only if you are alert as THYROCAB 5MG TABLET may cause dizziness.
Uses of THYROCAB 5MG TABLET
Directions for Use
Key Benefits
THYROCAB 5MG TABLET contains Carbimazole, an anti-thyroid agent used for the treatment of hyperthyroidism. It decreases the production of thyroid hormones by the thyroid gland. Thus, it balances the levels of thyroid hormones.
Storage
Drug Warnings
If you are known to be allergic to THYROCAB 5MG TABLET or any other anti-thyroid medicines, please tell your doctor. THYROCAB 5MG TABLET is not recommended for children below 2 years of age. If you are breastfeeding, avoid taking THYROCAB 5MG TABLET as it may be excreted in breast milk in small amounts and harm the unborn baby. Please consult a doctor if you are pregnant or planning for pregnancy before taking THYROCAB 5MG TABLET. You are recommended to use effective contraceptive measures while taking THYROCAB 5MG TABLET to avoid pregnancy. If you require radio-iodine treatment, you may be advised to stop taking THYROCAB 5MG TABLET temporarily. Drive only if you are alert as THYROCAB 5MG TABLET may cause dizziness. If you notice light coloured stools, yellowing of eyes or skin, tiredness, stomach pain, dark urine or loss of appetite, please consult a doctor immediately as these might be signs of liver problems.
Drug-Drug Interactions
Drug-Drug Interactions
Login/Sign Up
Drug-Food Interactions
Drug-Food Interactions
Login/Sign Up
Diet & Lifestyle Advise
- Avoid caffeine-containing drinks and foods such as regular coffee, black tea, regular soda, energy drinks, and black tea as they may worsen the symptoms of hyperthyroidism.
- Maintain a low iodine diet which includes egg whites, non-iodized salt, black coffee, tea, vegetable oils, honey, nut butter, unsalted nuts, sugar, jelly, jam, lemonade, fruits, moderate portions of chicken, beef, lamb, and turkey.
- Eat vegetables such as cauliflower, broccoli, Brussels sprouts, cabbage, mustard greens, radish, kale, and turnip roots.
- Eat foods rich in selenium like shrimp, beef, chicken, turkey, rice, eggs, cottage cheese, spinach, baked beans, and oatmeal as it helps to achieve normal thyroid levels more quickly.
- Avoid iodine-rich foods such as iodized salt, dairy products, iodine supplements, egg yolks, shellfish, and fish. Also, avoid soy sauce, soy milk, tofu, and soybean oil.
Side Effects of THYROCAB 5MG TABLET
- Headache
- Dizziness
- Nausea
- Skin rash
- Itching
- Joint pain
- Changes in taste
- Hair thinning
Habit Forming
Therapeutic Class
All Substitutes & Brand Comparisons
RX
Out of StockThyrodip 5mg Tablet
Lupin Ltd
₹189
(₹1.7 per unit)
99% CHEAPERRX
Out of StockThyrozole 5mg Tablet
Cadila Pharmaceuticals Ltd
₹20.6
(₹1.85 per unit)
99% CHEAPERRX
Carol-5 Tablet 120's
Eris Life Sciences Ltd
₹262
(₹1.97 per unit)
99% CHEAPER
Author Details
We provide you with authentic, trustworthy and relevant information
Drug-Diseases Interactions
Drug-Diseases Interactions
Login/Sign Up
FAQs
Drug-Drug Interactions Checker List
- WARFARIN
- THEOPHYLLINE
- PREDNISOLONE
- ERYTHROMYCIN
- DIGOXIN
- METOPROLOL
Special Advise
- Blood tests are recommended while taking THYROCAB 5MG TABLET to monitor your response to the treatment.
- Before restarting your treatment, your doctor may advise you on certain tests to check for bone marrow depression.
Disease/Condition Glossary
Hyperthyroidism: It is a condition in which the thyroid gland produces excessive thyroxine hormone. It increases the body’s metabolism and causes unintentional weight loss. The most common cause of hyperthyroidism is Grave’s disease (autoimmune disease) which occurs mostly in women. Other causes include excess iodine, inflammation of the thyroid gland, tumors of tests or ovaries, benign tumors of the pituitary gland or thyroid, or if large amounts of tetraiodothyronine are taken through dietary supplements. The symptoms include unexpected weight loss, irregular or rapid heartbeat, irritability, and sweating. Hyperthyroidism can be treated by medication, radioactive iodine, and sometimes surgery.

Have a query?
Alcohol
Safe if prescribed
The interaction of THYROCAB 5MG TABLET with alcohol is unknown. Please consult a doctor before consuming alcohol while using THYROCAB 5MG TABLET.
Pregnancy
Consult your doctor
Please consult a doctor if you are pregnant. THYROCAB 5MG TABLET is given to pregnant women only if the doctor thinks benefits outweigh risks.
Breast Feeding
Consult your doctor
Avoid breastfeeding while taking THYROCAB 5MG TABLET as it may be excreted in human milk in small amounts. Therefore, please consult a doctor if you are breastfeeding.
Driving
Safe if prescribed
THYROCAB 5MG TABLET may cause dizziness in some people. So, drive only if you are alert after taking THYROCAB 5MG TABLET.
Liver
Consult your doctor
THYROCAB 5MG TABLET should be given with caution, especially if you have a history of Liver diseases/conditions. The dose may be adjusted by your doctor as required. Avoid taking THYROCAB 5MG TABLET if you have a severe liver disorder.
Kidney
Consult your doctor
THYROCAB 5MG TABLET should be given with caution, especially if you have a history of Kidney diseases/conditions. The dose may be adjusted by your doctor as required.
Children
Safe if prescribed
THYROCAB 5MG TABLET is not recommended for children below 2 years as the safety and effectiveness were not established.